Body
Get to know your body through a better understanding of your anatomy and find the answers to some of your most common questions.

This is the second resource in our series on vaginismus. For a deeper dive into what vaginismus is, including its various types and causes, click here.
Part of the journey of healing from vaginismus is teaching your body that sex is safe, that your defense mechanisms no longer serve you, and that it is time to let them go.
Vaginismus can be effectively managed, and many women have found relief through various treatments, whether it’s pelvic physical therapy, psychotherapy, medical interventions, or a combination of these approaches. Here’s an overview.
Understanding vaginismus is the first step towards treatment. Counseling can help you understand what might have caused the condition and the treatment process. It can also address any emotional or psychological factors contributing to vaginismus, such as fear, anxiety, or past trauma.
A physical therapist specializing in pelvic floor issues can offer targeted exercises and techniques to relax and stretch the pelvic muscles. This can be particularly helpful in cases where vaginismus is related to physical conditions.
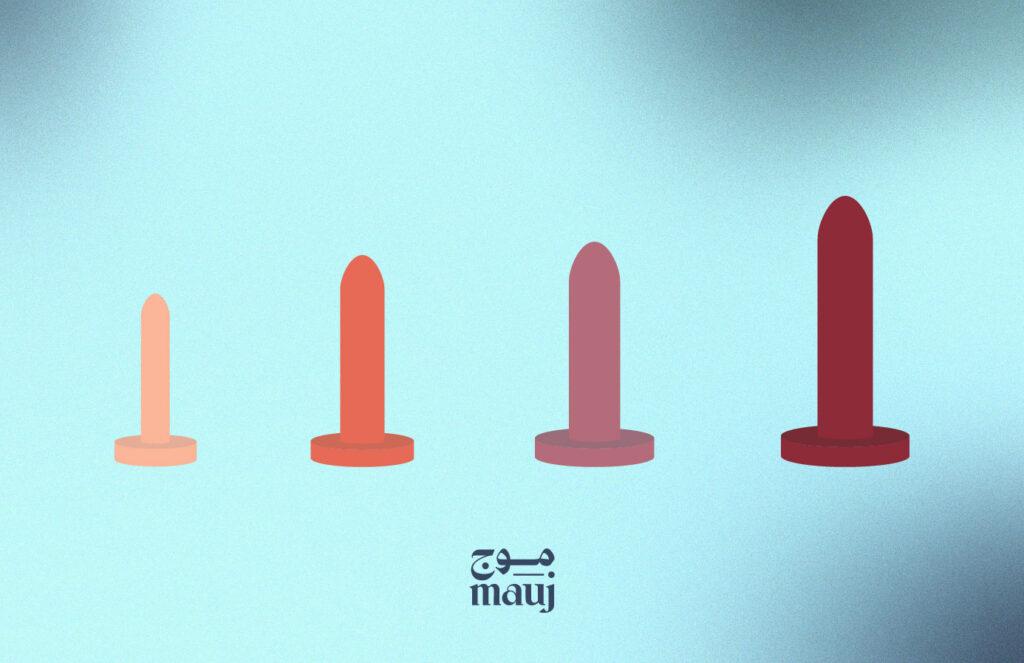
Vaginal dilators are medical devices used to gradually stretch the vaginal walls. Starting with the smallest size, a woman can slowly progress to larger sizes as she becomes more comfortable, helping to reduce muscle tension and anxiety about penetration. This is what they may look like:
This therapy involves learning to relax the vaginal muscles voluntarily through a combination of exercises and the use of vaginal dilators. It allows the woman to become more comfortable with insertion and reduces the reflexive tightening of the vagina.
CBT focuses on changing thought patterns and behaviors that contribute to the symptoms of vaginismus. If sex was portrayed negatively during our childhood (this includes being told it's dirty, shameful, or painful), these beliefs can become internalized, leading us to consciously or subconsciously fear the experience. CBT is particularly effective in addressing these deep-seated beliefs.
While there are no specific medications for vaginismus, doctors may prescribe muscle relaxants, pain relievers, or anti-anxiety medications to help ease symptoms during the treatment process.
In some cases, Botox injections into the pelvic floor muscles can temporarily relieve muscle spasms. This treatment is usually considered when other treatments have not been successful. It should also be noted that this is a temporary solution and doesn’t address the root cause.
Surgery is rarely recommended for vaginismus but may be considered in very severe cases where all other treatments have failed. The procedure, called a “vestibulectomy,” involves removing painful tissue from the entrance of the vagina.
Please remember: the options listed above do not constitute medical advice or direct recommendations but serve as an overview of potential treatments that must be discussed and prescribed by a healthcare professional.
A Final Note
If you're grappling with pain during sex but aren’t sure if it's vaginismus, read "Why Does Sex Hurt?" which delves into potential physiological and psychological factors that may contribute to painful intercourse. Remember, seeking support and understanding is a crucial step towards reclaiming control of your sexual health.
A recurrent or persistent involuntary spasm of the vaginal muscles, which interferes with sexual intercourse, making penetration difficult or painful for women. While it manifests as a physical symptom, it’s a psychological condition linked to a fear of penetration.
A procedure that involves carefully removing the painful or sensitive tissues of the vestibule, the area at the entrance of the vagina.
Did you find the answer you were looking for? Is there something we missed? What did you think of this resource? We want to hear from you.
